 |
 |
 |
 |
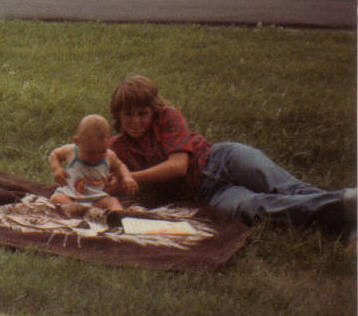
| My first summer of life was spent on the farm playing with Cindy. (July 1984) | Cindy was so excited to be getting married! (September 25, 1999) | She had me and my mom, Brenda, serve as bridesmaids and my cousin Shana as the flower girl. | Before heading off to her Sophomore dance Cindy had time for a picture with me. (1989) |
"I'm twelve," I state with the confidence only a nine-year-old could have. Walking through the parking structure of UK Hospital, I look up at my mom, who has taught me for as long as I can remember that lying is wrong but who also goes through this routine every time we are about to enter a hospital. Making sure that I, her nine-year-old daughter, knows to tell any of the nurses, should I be asked, that I am in fact twelve so that I will be allowed to visit the floor. Leading the way through a hospital that I know like my own backyard, I tell my mom about my day at school and what homework I have. My chatter quiets as I approach the solid wooden door. Pushing the heavy door out of my way, I tiptoe into the dimly lit room. The only light I have to maneuver my way around the bed comes from a muted TV and blinking lights from machines poked into the arms and through the nose of the fragile figure on the bed. I gently ease myself onto the edge of the bed, careful not to pull loose an IV or tube that will set off a parade of alarms from the blinking machines. In the dark, I silently watch the soft rise and fall of my sleeping aunt's chest as she flutters to wake from the touch of my small fingers. A smile stretches across her swollen face as I slowly come into focus.
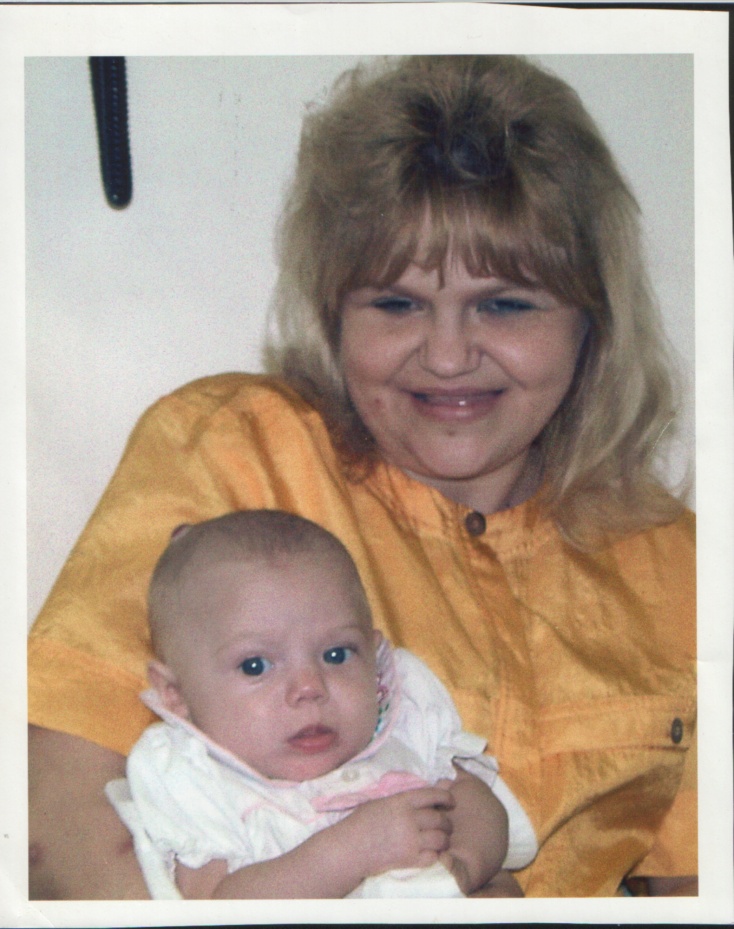
Looking back, I realize how sad it is that I've known what an IV does and that hospitals serve bad food and that if you're lucky a nice nurse might give you a Popsicle, since I was young. I didn't find it unusual that my aunt didn't go to school everyday; that some days teachers came to her house. And I found a sense of duty in going to retrieve her bottle of insulin from the refrigerator as she drew her own blood and gave herself a shot. You see my aunt was diagnosed with Type 1 diabetes at the ripe old age of seven, three years before I was born. Even with this debilitating disease my aunt, Cindy Claypoole Kuhlman, was a tremendous influence over my life. One of the first people to hold me after I was born, we shared a special bond; not so much that of aunt and niece but more so the unbreakable bond that connects sisters. As I grew up, she grew with me. We played Barbies, had sleepovers and art lessons and she even let me stay around when she had her older friends over; making sure to include me in her daily life as much as possible.
Unfortunately, my trips to the hospital were not an unusual occurrence and my aunt's situation is not unique. At the beginning of this century, 3-4 children per 1,000 required treatment with insulin due to Type 1 diabetes before the age of 20 (Gale para. 2). Type 1, or juvenile, diabetes is a disease that is most often diagnosed in children. With Type 1 diabetes the body does not make any or in some cases not enough insulin, which is the hormone that is needed to allow glucose to move from the bloodstream into the body’s cells to provide energy. Researchers have not yet found the cause of Type 1 diabetes. It is thought and there is much evidence to support the idea that the immune system of patients with Type 1 diabetes attacks and destroys insulin-producing cells in the pancreas, although it is not known why (Gale para. 28).
For people with diabetes to keep their disease under control they must follow a strict, well-balanced diet that includes very little, if any sugar. At the time that Cindy had diabetes, the only options for treatment were insulin tablets (taken by mouth) or insulin shots. Insulin was discovered 80 years ago and has greatly advanced since then (Shapiro para. 1). Around the time that my aunt was diagnosed with diabetes, the insulin pump was invented. The small-computerized pumps can be worn on a belt or carried in the patient’s pocket. A needle is inserted and taped in place to automatically deliver a steady dose of insulin throughout the day and night (Insulin para. 14). The insulin pump most closely simulates the way a body would normally release insulin and is therefore thought to enable the user to live a more flexible lifestyle. When she was 16, Cindy got an insulin pump to help control her blood sugar levels. The doctors felt that since she was on the go so much more than she had been when she was younger it would be a good idea for her to start using a pump instead of injections.
However, even with the medications available today not all diabetics are able to keep their disease under control. In some cases, a person’s blood sugar levels will rapidly increase or decrease without any apparent cause and there is no way to control this change. When a diabetic has erratic blood sugar levels over a long period of time, damage and disease of some other organs can occur. Some concerns diabetics may be faced with include higher risks for: heart attack, stroke, poor circulation, blindness, kidney failure/complications, neuropathy (nerve damage), skin disorders, foot problems (often resulting in amputation), gum disease and other mouth-related problems (Diabetes para. 1). After her transplant, Cindy wrote out some of her experiences with diabetes and the transplant process. She could best describe some of her complications and resulting surgeries in her own words:
At eleven years old I began having severe complications with my diabetes: nerve and circulation failure, which caused an enlarged bladder; and diabetic retinopathy which is damage done to the blood vessels in my eyes. I had three laser treatments on each eye and three surgical procedures because the laser treatments caused scar tissue that pulled on the retina of my eye. With all this amazing medical technology, I still lost the vision in my right eye. Other problems included gastroperesis (major difficulties digesting food properly), which meant medications and limiting my diet, erratic blood sugar levels, which led to a coma state for a matter of minutes at one time in May 1996, high blood pressure, bone infections, urinary tract infections and renal failure (my kidneys were not working on their own), which caused me to have to catheterize myself to be able to urinate.
The only cure for diabetes is a pancreas transplant. Often kidney damage due to diabetes is so severe that a kidney transplant is also necessary for the patient’s livelihood. Unfortunately, not all diabetics are able to receive a needed transplant due to the fact that so few organs are available. As of February 24, 2003, 80,448 people in the United States were waiting for an organ transplant. Of the 80,448 people in the United States waiting for one or more organs to become available for transplantation, 621 of these people live in Kentucky. Twenty-two of those people in Kentucky on the waiting list are waiting for a kidney and pancreas to become available (OPTN para. 1).
Due to the fact that so many people are waiting for organs and that organs are in such short supply, the number of people that are placed on the waiting list must be limited. To limit numbers and to help assure the success of a transplant, possible candidates must go through extensive medical and psychological testing. In August of 1995, Cindy’s doctors began to discuss the possibility of transplantation due to kidney and pancreas failure. After much research, thought, prayer and discussion with family, friends and other transplant recipients she decided to go for the testing to see if she qualified to be placed on the list to receive not only a new pancreas but also a kidney. Cindy was more than willing to explain the testing process she had to go through to be placed on the list, she described her experiences as follows:
On August 16,1995, I began the testing... if you can think of it, I was probably tested for it, everything from running dye through my veins, being required to collect frequent twenty-four hour urine specimens, tissue matching, having blood drawn and tested on a constant basis, and many EKGs, x-rays and CAT scans. I also under went a psychological examination to see if I could handle the stress related to a transplant. I was placed on the K.O.D.A. (Kentucky Organ Donation Association) list a little over one year after the testing had started, on September 3, 1996.
What followed was an extremely stressful time, not only for my aunt but also for the family as a whole. Every time the phone rang we would jump, hoping that it was news that Cindy was on the way to the hospital for her transplant. I think that the five months of waiting was one of the hardest things we had to go through; not knowing if an organ match would be made was heart-breaking. It’s hard to tell how many possible matches were missed in that time because the person wasn’t an organ donor or because they hadn’t informed their family of their decision to become a donor. Many people make the mistake of believing that if they have signed the back of their license they are automatically organ donors in the event of their death. However, this is not true, your family must be informed of your decision and must give consent for you to become an organ donor in the event of your death.
February 4, 1997, 12:35 a.m.: waking up from a peaceful dream to a ringing phone, I made my way across my bedroom to the phone. Still in a dream state, I answered with a barely audible, “Hello?” Waiting at the other end of the phone for me was the much-anticipated news. My aunt’s voice was spilling with emotion, both excitement and nervousness among the thousands of other feelings barreling through her head. She had just hung up with a K.O.D.A. representative that had called to tell her that she needed to arrive at the University of Kentucky Hospital (a two hour drive) as soon as she could. I don’t know how I managed to convince my legs to carry me down the stairs to get my mom to pick up the phone for news of her sister’s second chance at life.
By 6:30 a.m. Cindy was being prepped for surgery. After, a few last minute tests; two doses of anti-rejection drugs and steroids were given to her and she was wheeled into surgery at 9:40 a.m. We were told the surgery could last up to eighteen hours. That day, my mom sent me to school because she knew we had a long wait ahead and there was nothing I could do at the hospital. I don’t think that I was in the same universe as my 7th-grade friends all day; my mind was with my aunt and her team of surgeons. Eight and a half hours after being brought into surgery Cindy was in recovery with a new kidney and pancreas.
The following five weeks were spent in the hospital with some complications. My after school routine often involved visiting my beloved aunt in the hospital and watching her strength slowly grow. The surgery was a success and Cindy was no longer a diabetic. Without the need to take insulin, Cindy’s new daily routine included anti-rejection pills that she would have to take for the remainder of her life.
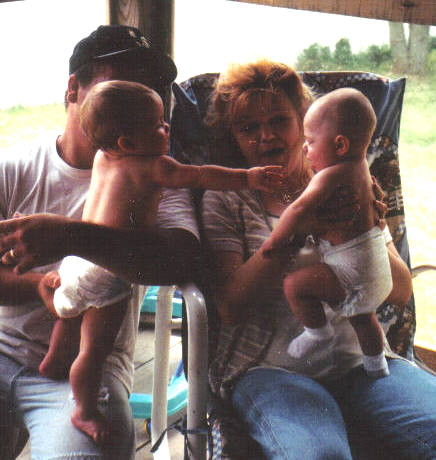
Following the transplant, Cindy’s quality of life improved beyond belief. In September of 1999, she married her boyfriend of six years. On January 28, 2000, the day before she turned 27; my aunt gave birth to our family’s “miracle baby”. We consider Delaney Lorraine, our miracle baby because she was born against all odds. Not only was Cindy told from the age of twelve that she would never be able to have a baby but if she hadn’t been given the gift of life by a complete stranger, there is no way that she would have been healthy enough to have this beautiful little girl.
Delaney is truly a blessing to our family. Cindy was glowing with pride and happiness every time I saw her. She was excited to buy her first house with her brand new family. She had so many ideas for redecorating her house and raising Delaney. It was amazing to see the sickly girl I grew up with turn into the happy and healthy woman she did after her transplant.
Unfortunately, someone had to lose his or her life for Cindy to have a second chance at hers. However, that person would have passed away whether or not he was an organ donor. The donor and their family had the chance to give total strangers the most valuable gift of all and through their own personal tragedy were able to provide a miracle to another family. Not just that of a second chance of life for one woman but a first chance at life for her baby.
My family and I lost Aunt Cindy eight months after she gave birth to Delaney on October 11, 2000 due to complications with rejection. Losing Cindy has had a devastating effect on my family. Although no one could ever take her place, having Delaney has been a great comfort to all of us. Watching Delaney bite her tongue as she performs difficult tasks and hearing her laugh brings images of my aunt running back into my mind. At the age of three, Delaney has shown no signs of diabetes. She is a healthy, intelligent and well adjusted little girl that loves to look at pictures of her Mommy.
To date, 1,634 people have donated organs in Kentucky; resulting in 3,404 transplants. 1,150 of those donors were deceased and the final decision of whether or not to donate was made by the donors’ family (OPTN para. 1). The decision to donate is a very personal one that everybody should make for his/her own self and express to their family. In the event of your death, you will not be available to express your wishes, so your family will be asked to make the ultimate decision. Many people never consider the possibility of their own death at an early age; let alone whether or not they wish to become organ donor. Of the deceased organ donors in Kentucky, 362 of them were from the ages of 18 to 34 and another 284 were between the ages of 35 and 49 (OPTN para. 1). These age groups include many people that might be reading this. It’s important that you consider the possibility of becoming an organ donor now so that if it comes down to it your family will not have to make the decision for you because it is too late.
When considering becoming an organ donor many people have questions and concerns must be answered before they can make their decision. With so many myths concerning donation, it is important to make sure that you get the facts right before making your own decision. In regard to the question of whether or not your religion prohibits donation: while every religion has various views on specifics, most major religions of the world permit, allow and support organ transplantation and donation (Does para. 34). Another concern that many people have is the question of whether their donation will cost their family money. This is never the case! Your family will not be required to pay for your donation after death. Many people are also worried that they will not be able to have an open casket funeral if they donate their organs. The process of donation is just like any other operation; your body is treated with respect at all times. There is no reason that a person wouldn’t be able to have an open-casket funeral due to donation. Many senior citizens think that they are too old to donate their organs. To date, 42 people in Kentucky over the age of 65 have become organ donors after death but with education of this age group this number could greatly improve. 234 people between the ages of 50 and 64 have been donors in Kentucky and although this number is fairly high in comparison to some other age groups, it would be great to improve it also! With higher numbers of donors more people will be able to receive transplants, which means that more lives will be saved!
Everyday approximately 102 people are added to the transplant list but only 63 people from the list receive a transplant in that same day. Because these numbers are so lopsided, sixteen people die everyday while waiting for an organ to become available. These deaths should not take place! People in this country, that could be organ donors and that could save lives with their donation, die everyday. After death you have no use for your organs, why not give them to someone who could use them instead of having them go to waste being buried with you? One organ donor can save or enhance the life of up to fifty people! So please make and share your decision with your family to give life in the event of your death.
Everyday my family thanks God, the family of the donor and the person who donated their organs for the three years with a healthy and happy Cindy. We know that without that person we wouldn’t have had the extra time with Cindy and we most definitely would not have our Laney Lou to brighten everyday without Cindy.
 |
 |
 |
 |
| Cindy holding Laney and my Uncle John holding his daughter Megan. (June 2000) | Laney loves to swing! (June 2000) | Cindy showing Delaney to her one of her transplant doctors, Dr. Ranjan. (April 2000) | Laney Lou was so excited about the snow this year! (December 2002) |
What does my religion say about organ donation and transplantation?
Where can I find out more about donation myths and the real facts?
Can I find more information about becoming a donor online? (This also has a printable donor card)
Where can I find more information about Type 1/Juvenile Diabetes?
 |
 |
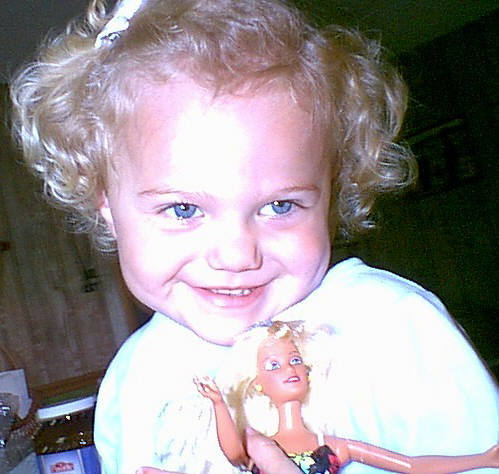 |
| Laney likes to wear cowboy hats as much as Cindy did. (October 2001) | Laney and Megan love spending time together. (January 2002) | Laney shares the same love for Barbie Dolls that Cindy and I had. (June 2002) |
“Diabetes Complications and Related Concerns.” American Diabetes Association. 18 Feb. {2003 http://www.diabetes.org/main/application/commercewf?origin=*.jsp&event=link(C3)}.
“Donation Statistics.” Home page. 2003. Coalition on Donation. 23 Feb. 2003. {www.shareyourlife.org/fact_stats.html}.
“Does My Religion Approve of Organ Donation?” Gallagher, Christine Comp. Home page. Transweb. 23 Feb. 2003 {http://www.transweb.org/qa/qa_don/religion.htm}.
Gale, Edwin. “The Rise of Childhood Type 1 Diabetes in the 20th Century.”
“Insulin Delivery.”
Shapiro, James. “Eighty Years After Insulin: Parallels with Modern Islet Transplantation.”